While falls prevention has become standard in inpatient care, injury prevention has gotten less attention, both in research and everyday practice. Injuries from falls can have serious consequences in patients, ranging from minor cuts and bruises to fractures, head injury, and even death. An estimated 11,000 patients die from falls in U.S. hospitals every year.
Injurious falls were deemed a healthcare-acquired condition (HAC) by the 2005 Deficit Reduction Act, and hospitals no longer receive reimbursement for treating injuries resulting from falls occurring during hospitalization. The average cost of treating injurious falls ranges from $24,000 to $27,000.
More recently, the Affordable Care Act led to changes in reimbursement models. These models factor in the occurrence of HACs, including injurious falls, to incentivize hospitals to improve patient outcomes. According to current projections, the annual financial burden of injurious falls will reach $47 billion by 2020.
Regulatory standards require hospitals to provide fall-prevention programs to patients at risk of falling. While these programs include care plans and protocols for preventing falls, they may fail to provide specific guidance or interventions for preventing injuries from falls.
Injury-prevention strategies and devices
Don’t confuse fall-prevention strategies and devices with injury-prevention strategies and devices. Bed and chair alarms, lap belts, gait belts, chair wedges, and nonslip footwear are designed to prevent falls, not fall-related injuries. Injury-prevention interventions are critical components of high-quality care. They include the use of material resources, such as floor matting or compliant flooring, hip protectors, low-low beds, and helmets or protective caps.
Special flooring
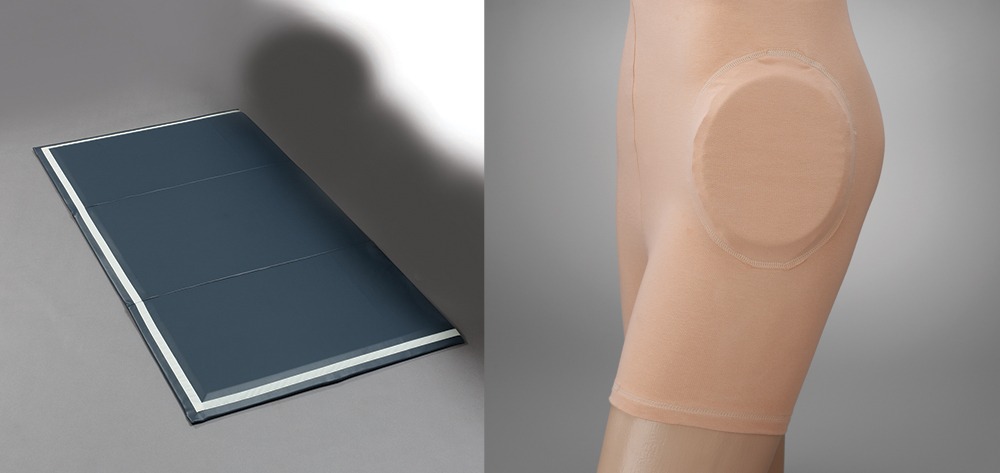
Compliant flooring and floor matting provide a cushioned surface that reduces impact, decreasing the likelihood of injury if the patient falls. Compliant flooring gives under pressure. This concept is relatively new and still uncommon in inpatient care settings.
Floor matting, on the other hand, has been used in practice for several years. A mechanical engineering study of floor matting showed it reduced injury by as much as 99%. Floor matting has several advantages:
- It offers protection from both fractures and head injury.
- It’s relatively inexpensive—usually less than $150.
- It’s reusable and easily cleaned between patient uses.
- It’s portable, transitioning from the bedside to placement in front of chairs or other areas when patients are mobilized out of bed.
Beveled matting is preferred because it’s less likely to pose a tripping hazard for nursing staff. Folding mats are preferred if storage space is scarce. (See Flooring that helps prevent injuries.)
To use floor matting effectively, staff must understand it should be placed only when the patient is left unattended. When staff members are working actively with the patient or the patient is being mobilized by staff, matting should be taken up and placed to the side.
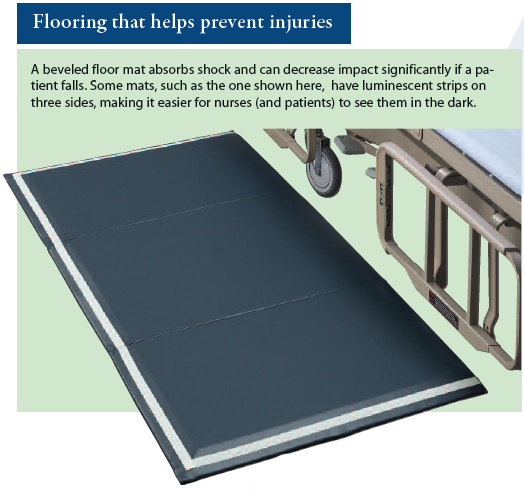
Hip protector
Hip protectors reduce impact from falls that could cause hip fracture. Available in briefs or pant-type options, these garments have protective pads or cushions around the lateral hip areas. They can be particularly effective for frail patients and those who have a degenerative bone disease or a low body mass index. They are inexpensive and can be stored easily in supply rooms. Although hip protectors are for single patient use, the patient can continue to wear them throughout care transitions, including discharge to the home. (See Protection against hip fractures.)
Low-low beds
Low-low beds keep the patient as low to the ground as possible, reducing impact if he or she falls from the bed. Many healthcare organizations use these beds on a rental basis, although owning them is becoming more prevalent. Be aware that low-low beds offer injury protection only if the patient falls directly from the bed.
Staff requires education to learn how to use these beds properly. When the bed is positioned all the way down, patients who are weak (especially in the quadriceps) may have trouble getting out of bed safely. Low-low beds should be raised to the appropriate height for each patient to allow safe transition out of bed.
Helmets and protective caps
Helmets and protective caps protect the head from impact during a fall. Several varieties are available, ranging from full head–hard shell helmets to vented foam helmets to caps with protective impact polymers. Cost varies by type, ranging from about $35 to $150.
These devices typically are for single-patient use. Like hip protectors, helmets travel well with the patient throughout care transitions. Helmets and protective caps can be particularly useful and effective in patients at risk for head bleeds secondary to coagulopathies. Head protection should be a serious consideration in patients who are receiving anticoagulants or have liver disease, elevated partial thromboplastin times, or low platelet counts secondary to oncologic therapies.
Right resource, right patient, right time
Knowing the purpose of each material resource and when and how to use it is crucial to implement these devices effectively in preventing and managing falls and injuries. Routine inservice education from vendors and standardized orientation of new staff to all devices used in patient care can improve compliance in their use. To standardize implementation of these resources, healthcare organizations should provide clinical decision support through care plans and protocols that address when to use appropriate material resources. Providing the right resource to the right patient at the right time is critically important.
Amy L. Hester is director of nursing research and innovation at the University of Arkansas for Medical Sciences Medical Center in Little Rock, Arkansas.
Selected references
Bowers B, Lloyd J, Lee W, Powell-Cope G, Baptiste A. Biomechanical evaluation of injury severity associated with patient falls from bed. Rehabil Nurs. 2008;33(6):253-9.
Currie L. Chapter 10: Fall and injury prevention. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. https://archive.ahrq.gov/professionals/clinicians-providers/resources/nursing/resources/nurseshdbk/CurrieL_FIP.pdf
Wu S, Keeler EB, Rubenstein LZ, Maglione MA, Shekelle PG. A cost-effectiveness analysis of a proposed national falls prevention program. Clin Geriatr Med. 2010;26(4):751-66.